FHIR4THIM - Data Model
Working Draft
- Latest version:
- http://iot.ee.surrey.ac.uk/tihm/models/fhir4tihm/ (JSON, CSV)
- Last Update:
- Date: 18:24:00 14/07/2016 BST
Authors: - Shirin Enshaeifar, Institute for Communication Systems, University of Surrey
- Payam Barnaghi, Institute for Communication Systems, University of Surrey
- Tarek Elsaleh, Institute for Communication Systems, University of Surrey
- Contributors:
-
to be included ...
- See Acknowledgements
- References:
- See Reference List
Abstract
Health Level-7 or HL7 refers
to a set of international
standards for transfer of clinical and administrative data between
software applications used by various healthcare providers.
HL7
specifies
a number of flexible standards, guidelines, and methodologies
by which various healthcare systems can communicate with each other.
Such guidelines or data standards are a set of rules that allow
information to be shared and processed in a uniform and consistent
manner.
In particular, the Fast Healthcare Interoperability Resources (FHIR) is a new standard from HL7 International designed to be easier to implement, more open and more extensible than other versions of HL7. FHIR leverages a modern web-based suite of API technology, including a HTTP-based RESTful protocol, HTML and Cascading Style Sheets for user interface integration, and a choice of JSON or XML for data representation.
Status of this Document
This is a work in progress and as such is subject to change. Comments are very welcome, please send them to First Author.
- Introduction
- UML Diagrams
- Simplified model: FHIR4TIHM
- JSON Examples using FHIR Standard
- Tools to Convert CSV2JSON using FHIR Standard
1. Introduction
FHIR is a healthcare information exchange standard that makes use of an HL7-defined set of "resources" to support information sharing by a variety of means, including documents, messages, services and RESTful interfaces. Thus, FHIR is suitable for use in a wide variety of contexts – mobile phone apps, cloud communications, server communication in large institutional healthcare providers, and much more.
FHIR defines resources for clinical and administrative content (e.g. Observation, Patient, Location, Organisation, etc.) as well as resources for infrastructure purposes. FHIR resources are small reusable structures where each resource has logical table, UML definition, and XML or JSON template.To exploit FHIR standard for the TIHM project, resources will be first represented using the UML diagrams in which elements are followed by their types and cardinalities. Thus, it is important to undesrand the concept of data types and cardinality prior to the UML diagrams.1.1 Types of elements
The FHIR specification defines a set of data types that are used for the resource elements. In general, data types are categorized into two groups: (i) primitive types which are single elements, and (ii) complex types which are re-usable clusters of elements. Lists of data types are summarized below:
|
Primitive data types: FHIR name |
Value Domain |
|
true | false |
|
|
A signed 32-bit integer (for larger values, use decimal) |
|
|
string: |
A sequence of Unicode characters.
|
|
Rational numbers
that have a decimal representation |
|
|
A Uniform Resource Identifier Reference. Note that URIs are case sensitive. |
|
|
An instant in time - known at least to the second and always includes a time zone. Note that this is intended for precisely observed times, i.e. this type is for system times, not human times. |
|
|
A date, or partial date (e.g. just year or year + month) as used in human communication. There is no time zone. |
|
|
A date, date-time or partial date (e.g. just year or year + month) as used in human communication. If hours and minutes are specified, a time zone SHALL be populated. Seconds must be provided due to schema type constraints but may be zero-filled and may be ignored. Dates SHALL be valid dates and the time "24:00" is not allowed. |
|
|
A time during the day, with no date specified. Seconds must be provided due to schema type constraints but may be zero-filled and may be ignored. The time "24:00" is not allowed, and neither is a time zone. |
|
code |
A value which is taken from a set of controlled strings defined elsewhere. |
id |
Any combination of alphabets ('A..Z' or 'a...z'), numbers ('0...9'), '-' and '.' upto 64 characters. |
|
Complex data types: FHIR name |
Value Domain |
|
This type is for containing or referencing attachments - additional data content defined in other formats. The most common use of this type is to include images or reports in some format such as PDF. |
|
Coding |
Coding is a representation of a defined concept using a symbol from a defined "code system". |
|
CodeableConcept
represents a value that is usually supplied by providing a reference to
one or more terminologies or ontologies, but may also be defined by the
provision of text. |
|
|
A numeric or alphanumeric string that is associated with a unique object or entity within a given system. Typically, identifiers are used to connect content in resources to external content available in other frameworks or protocols. |
|
|
A measured amount
or an amount that can potentially be measured. Quantity includes:
|
|
|
A set of ordered Quantity values defined by a low and high limit; i.e. Range specifies a set of possible values. |
|
|
A relationship between two Quantity values expressed as a numerator and a denominator. The most common example of this is where the ratio represents a unit cost, and the numerator is a currency (e.g. 50/$10). |
|
|
A time period defined by a start and end date/time. A period specifies a range of times. |
|
|
Specifies an event that may occur multiple times. Timing schedules are not used for recording when things did happen, but when they are expected or requested to occur. A Timing schedule can be a list of events and/or criteria for when the event is to happen, which can be expressed in a structured form and/or as a code. |
|
|
A name of a human with text, parts and usage information |
|
|
A postal address which is used to record a location that can be visited to find a patient or person. There are a variety of postal address formats defined around the world. |
|
|
Details for all kinds of technology-mediated contact points for a person or organization, including telephone, email, etc |
|
|
Data that comes
from a series of measurements taken by a device, with upper and lower
limits. There may be more than one dimension in the data. |
|
|
A Signature holds an electronic representation of a signature and its supporting context in a FHIR accessible form. |
|
|
A text note which also contains information about who made the statement and when. |
1.2 Cardinality
The notation for cardinality, used for attributes, are defines as below:|
cardinality value |
description |
|
0..1 |
No instance or just
one (optional, but no more than one) |
0..* or * |
Zero or more instances (optional, and any number of instances is allowed) |
|
1..1 or 1 |
Mandatory with
exatly one instance |
|
1..* |
Mandatory with at
least one instance |
2. UML Diagrams
To exploit the FHIR standard for THIM, we start with two major resources: Observation and Patient.2.1 Observation
Observations are central elements in healthcare, used to support diagnosis, monitor progress, determine baselines and patterns and even capture demographic characteristics. Most observations are simple name/value pair assertions with metadata, but some observations are multi-component observations. Some of the expected uses for the Observation resource include:- Vital signs: temperature, blood pressure, respiration rate
- Devices Measurements such as ECG data or Pulse Oximetry data
- Personal characteristics: height and weight
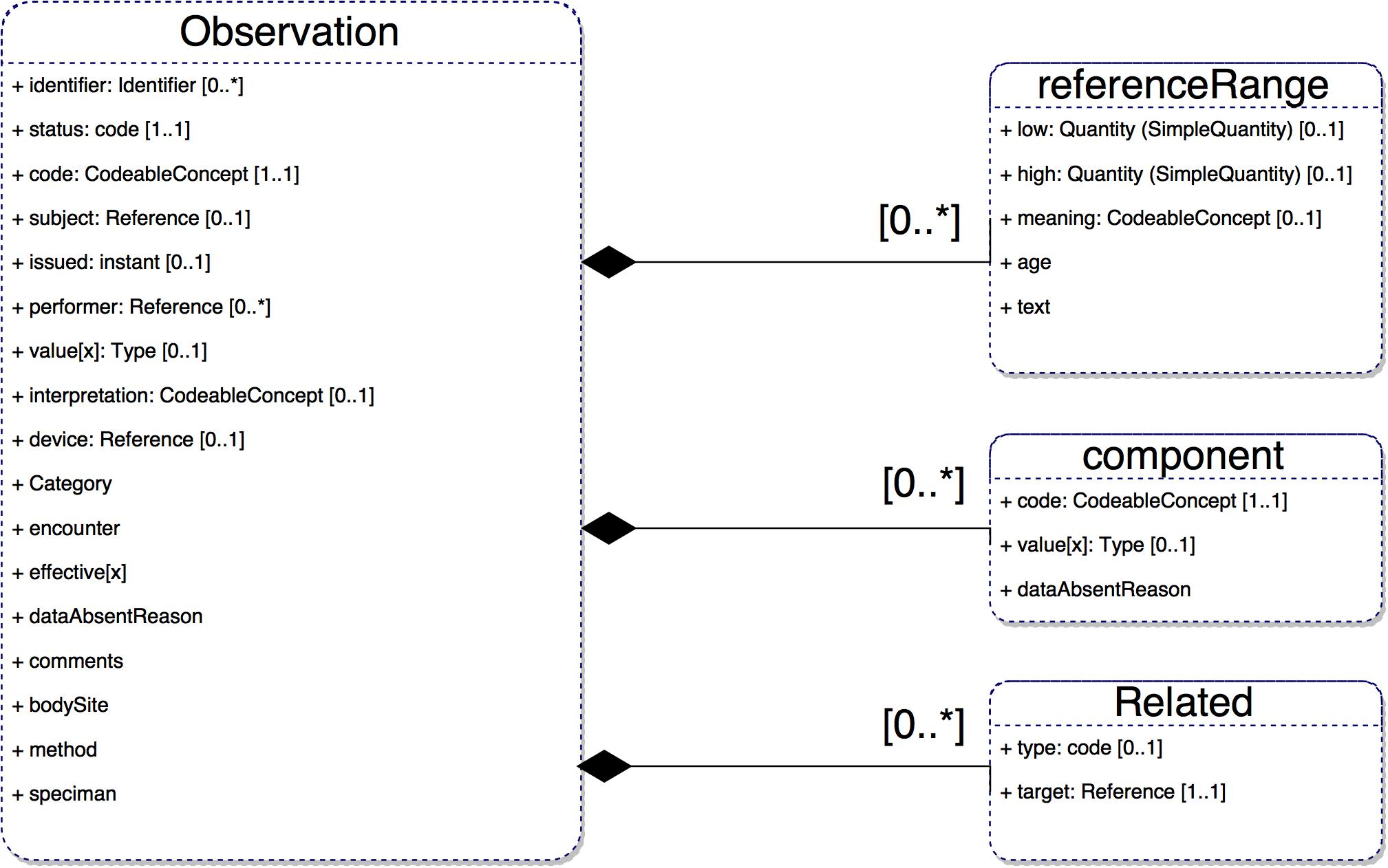
Brief descriptions for a subset of elements in the Observation resource are explained below:
|
Observation |
|
|
Definition |
Measurements and simple assertions made about a patient, device or other subject. |
|
Requirements |
Observations are a key aspect of healthcare. This resource is used to capture those that do not require more sophisticated mechanisms. |
|
Observation.identifier |
|
|
Definition |
A unique identifier for the simple observation instance. |
|
Requirements |
Allows observations to be distinguished and referenced. |
|
Observation.status |
|
|
Definition |
The status of the result value. |
|
Requirements |
Need to track the status of individual results. Some results are finalized before the whole report is finalized. |
|
Observation.code |
|
|
Definition |
Describes what was observed. Sometimes this is called the observation "name". |
|
Requirements |
Knowing what kind of observation is being made is essential to understanding the observation. |
|
Observation.subject |
|
|
Definition |
The patient, or group of patients, location, or device whose characteristics (direct or indirect) are described by the observation and into whose record the observation is placed. Comments: Indirect characteristics may be those of a specimen, fetus, donor, other observer (for example a relative or EMT), or any observation made about the subject. |
|
Requirements |
Observations have no value if you don't know who or what they're about. |
|
Observation.issued |
|
|
Definition |
The date and time this observation was made available to providers, typically after the results have been reviewed and verified. |
|
Observation.performer |
|
|
Definition |
Who was responsible for asserting the observed value as "true". |
|
Requirements |
May give a degree of confidence in the observation and also indicates where follow-up questions should be directed. |
|
Observation.value[x] |
|
|
Definition |
The information determined as a result of making the observation, if the information has a simple value. |
|
Quantity|CodeableConcept|string|Range|Ratio|SampledData|Attachment|time|dateTime|Period |
|
|
Requirements |
An observation exists to have a value, though it may not if it is in error, or it represents a group of observations. |
|
Comments |
Normally, an observation will have either a value or a set of related observations. A few observations (e.g. Apgar score) may have both a value and related observations (for an Apgar score, the observations from which the measure is derived). If a value is present, the datatype for this element should be determined by Observation.code. This element has a variable name depending on the type as follows: valueQuantity, valueCodeableConcept, valueString, valueRange, valueRatio, valueSampledData, valueAttachment, valueTime, valueDateTime, or valuePeriod. (The name format is "'value' + the type name" with a capital on the first letter of the type). If the data element is usually coded or if the type associated with the Observation.value defines a coded value, use CodeableConcept instead of string datatype even if the value is uncoded text. A value set is bound to the ValueCodeableConcept element. For boolean values use valueCodeableConcept and select codes from HL7 Version 2 Table 0136. These "yes/no" concepts can be mapped to the display name "true/false" or other mutually exclusive terms that may be needed. For further discussion and examples see the notes section below. |
|
Observation.interpretation |
|
|
Definition |
The assessment made based on the result of the observation. Intended as a simple compact code often placed adjacent to the result value in reports and flow sheets to signal the meaning/normalcy status of the result. Otherwise known as abnormal flag. |
|
Requirements |
For some results, particularly numeric results, an interpretation is necessary to fully understand the significance of a result. |
|
Observation.device |
|
|
Definition |
The device used to generate the observation data. |
|
Comments |
An extension should be used if further typing of the device is needed. Devices used to support obtaining an observation can be represented using either extension or through the Observation.related element. |
|
Observation.referenceRange |
|
|
Definition |
Guidance on how to interpret the value by comparison to a normal or recommended range. |
|
Requirements |
Knowing what values are considered "normal" can help evaluate the significance of a particular result. Need to be able to provide multiple reference ranges for different contexts. |
|
Comments |
Most observations only have one generic reference range. Systems MAY choose to restrict to only supplying the relevant reference range based on knowledge about the patient (e.g. specific to the patient's age, gender, weight and other factors), but this may not be possible or appropriate. Whenever more than one reference range is supplied, the differences between them SHOULD be provided in the reference range and/or age properties. |
|
Observation.component |
|
|
Definition |
Some observations have multiple component observations. These component observations are expressed as separate code value pairs that share the same attributes. Examples include systolic and diastolic component observations for blood pressure measurement and multiple component observations for genetics observations. |
|
Requirements |
Component observations share the same attributes in the Observation resource as the primary observation and are always treated a part of a single observation (they are not separable). However, the reference range for the primary observation value is not inherited by the component values and is required when appropriate for each component observation. |
|
Comments |
For a discussion on the ways Observations can assembled in groups together see Notes below. |
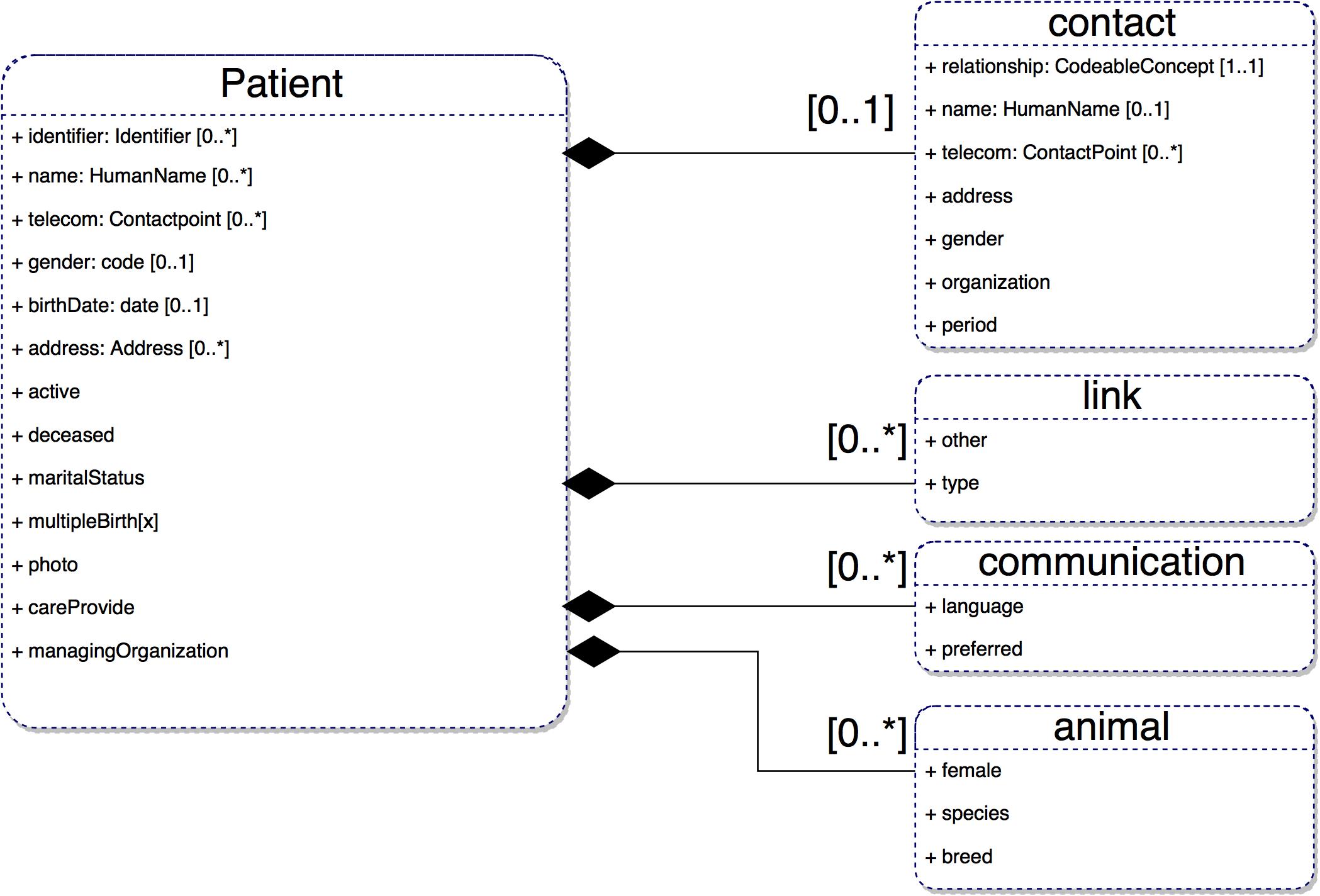
2.2 Patient
The Patient resource covers data about patients and animals involved in a wide range of health-related activities, including:
- Curative activities
- Psychiatric care
- Social services
- Pregnancy care
- Nursing and assisted living
- Dietary services
- Tracking of personal health and exercise data
|
Patient |
||
|
Definition |
Demographics and other administrative information about an individual or animal receiving care or other health-related services. |
|
|
Requirements |
|
|
|
Patinet.identifier |
||
|
Definition |
|
|
|
Requirements |
|
|
|
Patient.name |
||
|
Definition |
|
|
|
Requirements |
Need to be able to track the patient by multiple names. Examples are your official name and a partner name. |
|
|
Patient.telecom |
|
|
Definition |
A contact detail (e.g. a telephone number or an email address) by which the individual may be contacted. |
|
Requirements |
People have (primary) ways to contact them in some way such as phone, email. |
|
Patient.gender |
|
|
Definition |
Administrative Gender - the gender that the patient is considered to have for administration and record keeping purposes. |
|
Requirements |
Needed for identification of the individual, in combination with (at least) name and birth date. Gender of individual drives many clinical processes. |
|
Patient.birthDate |
|
|
Definition |
The date of birth for the individual. |
|
Requirements |
Age of the individual drives many clinical processes. |
|
Patient.address |
|
|
Definition |
Addresses for the individual. |
|
Requirements |
May need to keep track of patient addresses for contacting, billing or reporting requirements and also to help with identification. |
|
Patient.contact |
|
|
Definition |
A contact party (e.g. guardian, partner, friend) for the patient. |
|
Requirements |
Need to track people you can contact about the patient. |
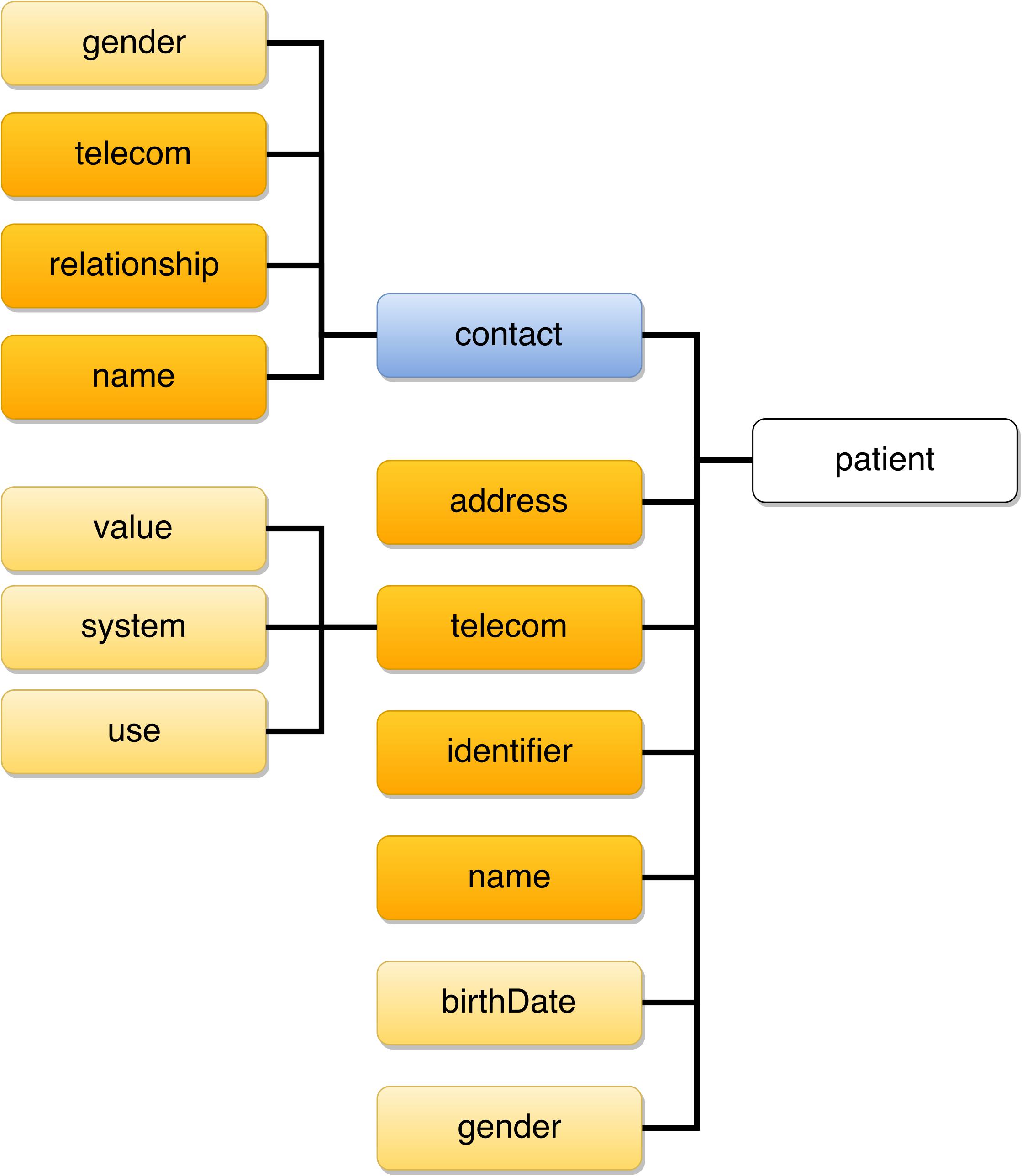
3. Simplified Model: FHIR4TIHM
In summary, Observation and Patient resources in the TIHM project can be represented using the following diagrams, in which:yellow block is a data type which describes an element that has a value attribute/property.
orange block is a data type which describes an element that has other elements.
red block is an element which can have one of a several different types.
blue block is an element that is part of the resource and has elements within it defines in the same resource or profile.
green block is an element that contains a reference to another resource.
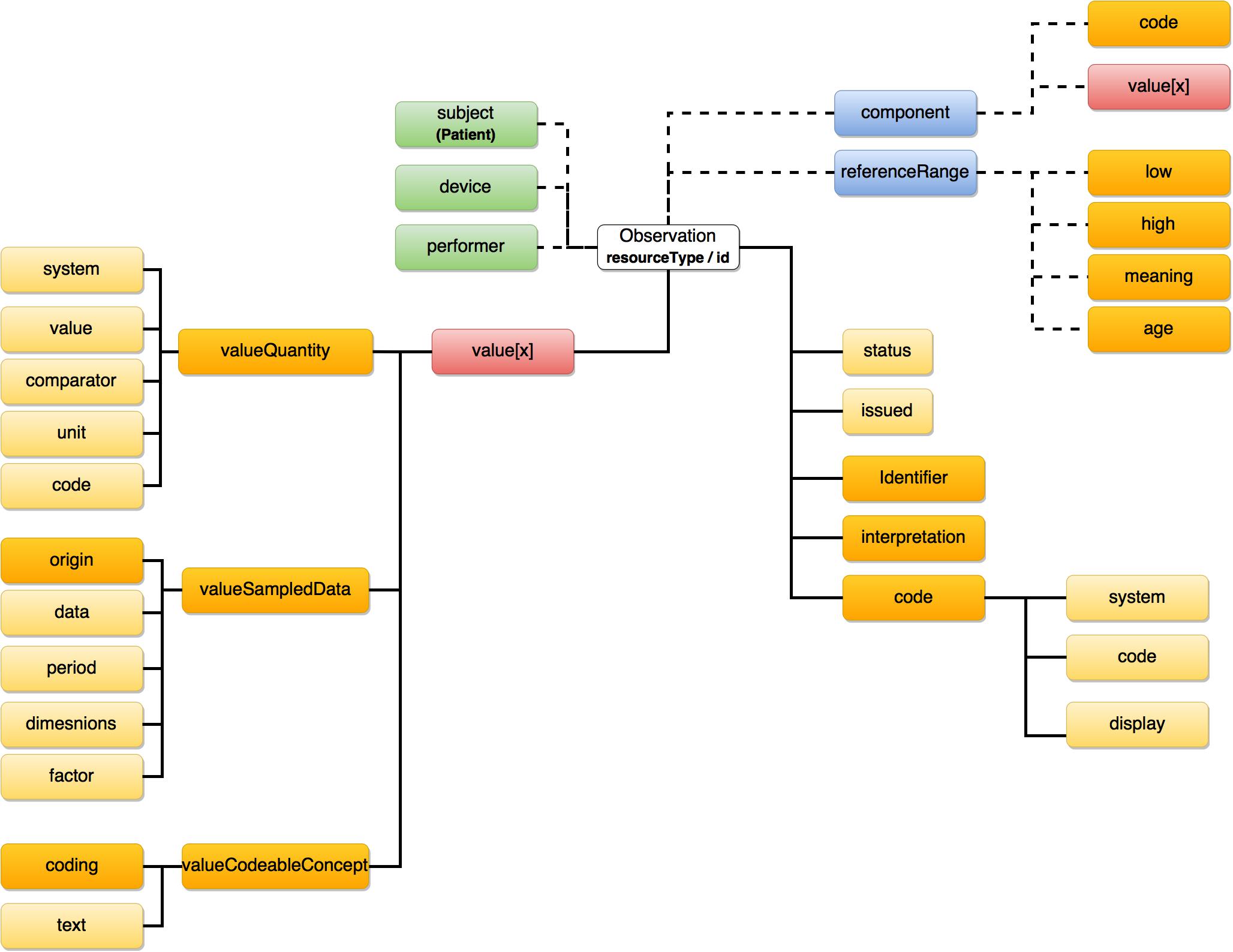
3.1 Best Practices
- value[x] / valueQuantity: Data which are represented as a single value, such as body/room temperature, weight, and humidity.
- value[x] / valueSampledData: Data that come
from a series of measurements taken by a device, e.g. ECG data.
- value[x] /valueCodeableConcept: Data that are represented using boolean values, such as motion detection alarms.
- Component / value[x] / valueQuantity: Data which have multiple component observations. These component observations are expressed as separate code value pairs that share the same attributes.These data includes systolic and diastolic blood pressure.
4. JSON Examples using FHIR Standard
{
"resourceType": "Bundle",
"type": "transaction",
"entry": [{
"resource": {
"resourceType": "Patient",
"id": "hca-pat-1",
"identifier": [{
"use": "usual",
"type": {
"coding": [
{
"system": "http://hl7.org/fhir/v2/0203",
"code": "MR",
"display": "Medical record number"
}
],
"text": "Medical record number"
},
"system": "http://hospital.smarthealthit.org",
"value": "hca-pat-1"
}],
"active": true,
"name": [{
"family": ["Smith"],
"given": ["John"]
}],
"gender": "male",
"birthDate": "01/01/1911",
"address": [{
"use": "home",
"line": ["5G/ICS UniS"],
"country": "UK"
}]
}
},{
"resource": {
"resourceType": "Observation",
"id": "hca-obs-weight",
"subject": {
"reference": "Patient/hca-pat-1",
"display": "Smith John"
},
"code": {
"coding": [{
"system": "http://lonic.org",
"code": "3141-9",
"display": "Weight Measured"
}],
"text": ""
},
"valueQuantity": {
"value": 5,
"unit": "lbs",
"system": "http://unitsofmeasure.org",
},
"status": "final",
"reliability": "ok"
}
},{
"resource": {
"resourceType": "Observation",
"id": "hca-obs-blood pressure",
"subject": {
"reference": "Patient/hca-pat-1",
"display": "Smith John"
},
"code": {
"coding": [{
"system": "http://loinc.org",
"code": "55284-4",
"display": "Blood pressure systolic & diastolic"
}],
"text": ""
},
"valueString": "112-85",
"component": {
"code": {
"coding": [{
"system": "http://loinc.org",
"code": "8480-6",
"display": "Systolic blood pressure"
}],
},
"valueQuantity": {
"value": 112,
"unit": "mm[Hg]",
"system": "http://unitsofmeasure.org",
},
"code": {
"coding": [{
"system": "http://loinc.org",
"code": "8462-4",
"display": "Diastolic blood pressure"
}],
},
"valueQuantity": {
"value": 85,
"unit": "mm[Hg]",
"system": "http://unitsofmeasure.org",
}
},
"status": "final",
"reliability": "ok"
}
}
]
}
5. Tools to Convert CSV2JSON using FHIR Standard
5.1 CSV2FHIR-v1
To generate a common data model for TIHM project, we have developed a Python program to map a CSV file into the JSON format which complies the FHIR specification. Our developments were inspired by this link. Note that two major resources (i.e. Observation and Patient) are considered in the current version, and more resources may be added over time.
The current CSV file includes one column per observation, however, this will be modified in our future version to enhance the extendablity and interoperability.
5.2 CSV2FHIR-v2
Will be added soon.Acknowledgements
This work is part of Technology Integrated Health Management (TIHM) project at the Institution for Communication Systems University of Surrey.